What is the pancreas?
It may not be an organ that is talked about much, but the pancreas plays the important role in ensuring that food that's digested well, and regulating our blood-sugar levels. It is located in your abdomen, behind your stomach.
What does the pancreas do?
The pancreas has 2 main functions.
Firstly, it produces digestive enzymes – the biological molecules that help in the digestion of food. This allows the food we eat to be broken down and efficiently absorbed by the small intestines.
The pancreas is also responsible for producing hormones such as insulin and glucagon, which regulate blood-sugar levels in the body. Insulin helps lower the body's blood sugar when it gets too high, and glucagon raises blood sugar when it gets too low.
What is pancreatitis?
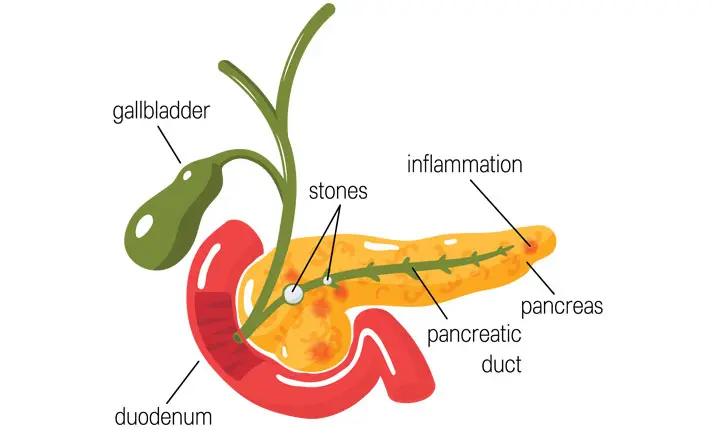
Pancreatitis is a condition that happens when there is inflammation of the pancreas. It can be acute or chronic.
Acute pancreatitis occurs when the pancreas suddenly becomes inflamed, leading to severe abdominal pain. The severity of acute pancreatitis can vary from mild to life threatening.
Chronic pancreatitis occurs when the pancreas is repeatedly inflamed over an extended period of time, usually several years. In severe cases it can result in impairment of digestion, as well as diabetes.
What causes pancreatitis?
There are many different conditions which can the pancreas to get inflamed and cause pancreatitis. The most common of which are gallstones and alcohol.
Other causes include:
- Related to procedures, such as Endoscopic Retrograde Cholangiopancreatography (ERCP)
- Excessive alcohol consumption
- Side effects of medication
- Cystic fibrosis
- Gallstones
- Hypercalcemia (high levels of calcium in blood)
- High triglyceride levels (a type of fat in the blood)
- Viral infections
- Trauma
- Cancer of the pancreas
What are the symptoms of pancreatitis?
The causes of pancreatitis may be varied, and the symptoms that point to the condition may differ depending on whether the pancreatitis is acute or chronic.
The symptoms associated with acute pancreatitis include:
- Severe pain in your upper abdomen, often spreading to the back
- Pain in the abdomen after eating
- High fever
- High pulse rate
- Feeling nauseous
- Vomiting
For chronic pancreatitis, patients may experience:
- Unintended weight loss
- Fatty stools (light-coloured and foul-smelling)
- Jaundice (yellowish discolouration of the eyes)
When should you see a doctor?
Should constant pain in the abdomen be experienced, consider making an appointment with a gastroenterologist for a detailed medical examination and diagnosis of potential medical conditions.
However, should the pain be so severe that you are unable to sit still or rest comfortably, seek immediate medical attention at your nearest emergency department.
How is pancreatitis diagnosed?
Should the gastroenterologist suspect pancreatitis, they may order the following tests to accurately diagnose the condition.
Blood tests
Acute pancreatitis can be detected by looking for elevated levels of amylase, which is one of the pancreatic enzymes.
Stool tests
Stool test results that reveal a high percentage of fat could mean that the digestive system isn't absorbing nutrients adequately – a sign of chronic pancreatitis.
Imaging scans may also be ordered to look for inflammation of the pancreas and the cause of the pancreatitis.
These include:
Computerised tomography (CT) scan
CT scans will be able to show the degree of inflammation in your pancreas and also exclude other causes of severe abdominal pain.
Abdominal ultrasound
This is useful for gallstone detection, which is one of the most common causes of pancreatitis.
Endoscopic ultrasound
This endoscopic procedure makes use of ultrasound imaging to detect structural abnormalities in the pancreas or bile duct which can cause pancreatitis.
Magnetic resonance imaging (MRI)
An MRI scan looks out for anomalies in the pancreas, pancreatic duct, bile duct as well as gall bladder.
How is pancreatitis treated?
Many of the treatment measures of acute pancreatitis are supportive, allowing time for pancreas to heal on its own. Some causes such as bile duct stones may require additional special endoscopic procedures as treatment
Pain control
Patients will be given pain medication to manage the severe pain that may be experienced with inflammation of the pancreas. Pain can also be alleviated in chronic cases through endoscopic ultrasound or radiological procedures to impede the nerves that that send pain signals.
Fasting
Eating often aggravates the severe abdominal pain from acute pancreatitis, hence patients may have to undergo fasting for a short period of time. Once the pain improves, they may be started back on a controlled diet that often features liquids first before solids.
Intravenous (IV) Drip
Patients may be admitted and put on an intravenous (IV) drip in the hospital to ensure that the body has enough hydration as patients are often fasted in the beginning and may also experience vomiting from the pancreatitis.
Endoscopic procedures
If a patient's pancreatitis is caused by stones in the bile or pancreatic ducts, or a narrowing of the pancreatic duct, ERCP may be needed to remove the stones or widen the duct.
During an ERCP, the surgeon will use an endoscope, a long, flexible tube that has a light and camera attached at the end, to examine the inside of the patient's bile duct and/or pancreatic duct. This is the preferred method of treatment of bile duct stones as no incisions need to be made in the skin.
Radiological procedures
Sometimes in cases of severe pancreatitis, tubes may have to inserted through the skin under x-ray guidance for drainage of fluid collections or pus around the pancreas.
Surgery
Surgery is often not required in the initial management of acute pancreatitis. However, in cases of severe pancreatitis, where tubes placed radiologically are unable to drain fluid or pus sufficiently, surgery may still be required for adequate drainage.
After acute pancreatitis has resolved, the surgeon may also recommend the removal of your gall bladder if gallstones are the cause of the pancreatitis. This is to prevent recurrent episodes of acute pancreatitis.
In chronic pancreatitis, surgery may be required for control of chronic pain if other methods have failed. Either by removing stones in the pancreatic duct or by removing part of the pancreas.
Additional treatments
Chronic pancreatitis may require additional support. As pancreatitis disrupts the production of digestive enzymes, pancreatic enzyme supplements may be prescribed so that a patient can continue to digest food normally. These enzymes will have to be taken with every meal.
Can pancreatitis be avoided?
Pancreatitis can potentially be avoided with adjustments to one's lifestyle. In particular:
Abstaining from alcohol
Research has shown that "chronic alcohol consumption causes 17% – 25% of acute pancreatitis cases". It was also shown that people who consume 4 – 5 drinks a day are at increased risk of the disease.
Quitting smoking
Research has also shown a link between cigarette smoking and the development of pancreatitis. Therefore, quitting the habit can reduce your risk of developing chronic pancreatitis and pancreatic cancer.
Maintaining a healthy weight
Obesity increases the likelihood of developing gallstones, and consequently, pancreatitis.
Should pancreatitis be suspected, consult a gastroenterologist for an accurate diagnosis of your condition and the available treatment options.