A midlife crisis can hit us in our 40s and 50s. It is that phase in life when work security is established, family life is stable and there’s a yearning for something different. It is also during this period in our lives that the body begins to feel the strains of our yesteryears, and joints begin to ache.
Learn about your healthcare needs as you age and speak with any one of our specialists about any health concerns your family members may have.
Knee arthritis and joint pain
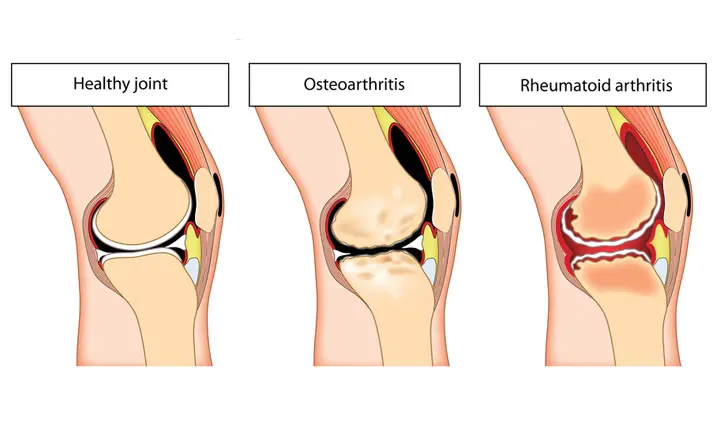
One of the most common causes of joint pain is arthritis. There are 2 major forms of arthritis – osteoarthritis and inflammatory arthritis (also known as rheumatoid arthritis).
Osteoarthritis
Osteoarthritis, the load-related wear-and-tear of the body’s joints, is more common and usually begins after age 40. The disease affects 35% of adults aged 65 and older and is the leading cause of mobility disabilities such as difficulty walking or climbing the stairs.
Inflammatory arthritis
Inflammatory or rheumatoid arthritis is an autoimmune disease that can occur in people of all ages. It is a systemic disease, which affects the entire body therefore, inflammatory arthritis can affect other organs, including the heart and lungs, in addition to the joints.
Knee osteoarthritis
The first sign of osteoarthritis in the knee is usually pain. This is most commonly felt at the front or sides of the knee with when climbing stairs or kneeling. As the condition progresses, even walking on flat ground can get affected.
Symptoms of knee osteoarthritis
Symptoms of knee osteoarthritis are more likely to develop over time. These include:
- Pain in the knees when getting up from a seated position or while climbing stairs
- Knee swelling or tenderness, which may be worse upon waking in the morning or after a period of inactivity
- Buckling or locking of the knee
- Sensation of grinding, or cracking or popping sounds when the knee bends and straightens (crepitus)
- Progressive stiffness or reduced range of motion, owing to pain, swelling or the breakdown of cartilage that makes it difficult to bend the knees smoothly
- Crookedness or deformity of the knees as muscles weaken and joint damage worsens
As joint damage cannot be reversed, it is important to seek advice early so that lifestyle changes and treatment can slow the progress of the disease.
Causes and risk factors of knee osteoarthritis
Knee osteoarthritis develops when the cartilage that cushions the knee joint wears away hence it is more common in older people. The following factors are associated with its development:
- Age, due to the gradual deterioration of cartilage, and the breakdown of muscle and connective tissues that support the knee joint
- Gender, as women are more likely to develop osteoarthritis, compared to men
- Family history of osteoarthritis
- Obesity, as increased weight places more pressure on the knee joint
- Repetitive stress on the knee joint, from work or sports
- Past injuries to the knee
- Congenital deformities or abnormalities of the joint or cartilage
- Certain metabolic conditions such as diabetes
How is knee osteoarthritis diagnosed?
To diagnose knee osteoarthritis, your doctor will take note of your medical history and perform a physical examination. This will include checking the affected knee for tenderness, swelling, flexibility and range of motion.
To confirm the diagnosis and rule out other possible causes, your doctor may also recommend imaging and/or laboratory tests such as:
- X-rays, which can reveal bone spurs and narrowing between the bones that indicates loss of cartilage
- Magnetic resonance imaging (MRI), to produce a detailed image of the bone and cartilage of the knee joint
- Blood tests, to rule out inflammatory or rheumatoid arthritis
- Joint fluid analysis, which involves drawing fluid from the joint to check for gout or infection
How is knee osteoarthritis prevented?
The right approach to preventing or slowing down the progression of knee osteoarthritis is in achieving a healthy body weight, being active, preventing injuries to your joints and seeking treatment early.
Keep a healthy body weight
Keeping a healthy body weight means avoiding being overweight. The less weight your knees have to bear, the less wear-and-tear they will have.
Avoid activities that may injure your joints
Some activities place additional stress on your knee joints. As much as possible, avoid excessive or prolonged squatting, kneeling and stair climbing. At the same time, try to maintain a healthy level of exercise and fitness.
Seek treatment early
Seeing a doctor early when you start to encounter knee pain can help to prevent joint pain or degeneration from getting worse. When small problems are treated early, and properly, you will have a better chance of recovering than if managed later.
How is knee osteoarthritis treated?
When you see a doctor for knee osteoarthritis, he or she will have 3 main avenues for treating you – medication, therapy or surgery.
Medication
Medicines for arthritis can be ingested, applied topically or injected into the knee.
Ingestible or oral medicines include painkillers that reduce pain but do not slow down the wear and tear of the joint. Supplements like glucosamine have been shown to slow down the progression of knee osteoarthritis.
Injectable medicines could be in the form of steroids for reducing pain and swelling, or joint lubricants that can reduce pain for up to 9 months.
Physiotherapy
Physiotherapy is sometimes needed to help patients regain knee mobility and strength. Your physiotherapist may also recommend wearing a knee guard or brace for additional support, to help reduce knee pain from osteoarthritis.
Surgery
The most daunting prospect for a patient with knee osteoarthritis is surgery. However, the right type of surgery, done at the right time by an orthopaedic specialist, has proven to be effective with very high rates of success.
Types of surgery can range from minimally invasive arthroscopy and cartilage transplantation to knee replacement.
Arthroscopy
Arthroscopy is a day surgery procedure and suitable for patients with mild osteoarthritis. Recovery is quick, with most patients able to walk comfortably the next day.
Some younger patients with more advanced osteoarthritis can benefit from cartilage restoration procedures.
There are various methods for restoring cartilage in the knee, ranging from arthroscopic procedures where the exposed bone is punctured to encourage new cartilage growth (microfracture), cartilage transplantation from new cartilage grown from the patient’s own cartilage (autologous cartilage transplantation), to grafting cartilage and bone from one part of the knee to another (osteochondral grafting). The choice of procedure and the success rate depends on an individual patient’s unique knee condition.
Knee replacement surgery
Knee replacement surgery is reserved for patients with advanced osteoarthritis. The procedure has come a long way since its introduction 50 years ago. Today, knee replacement patients are usually able to walk on the same day or a day after surgery. With the advancements in surgery techniques, the incisions are small and recovery is rapid. These developments also mean that knee replacement surgery now includes partial instead of total replacement, as well as more accurate surgery with custom designed instruments and computer guided surgery.
FAQs: Knee osteoarthritis
Does my diet have anything to do with arthritis in my knee?
Some patients with gout need to avoid certain foods, but the majority of patients actually do not have gout and do not need to follow a specific diet.
What supplements help prevent knee osteoarthritis?
Studies have shown that oral glucosamine can delay the progression of knee osteoarthritis but it has not been shown to prevent knee osteoarthritis in people who do not have the condition.